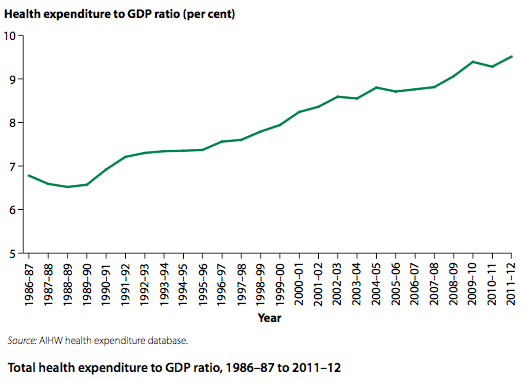
Health care expenditure versus expenditure on early intervention and prevention seeks to compare the treatment of disease and illness with prevention. For an effective health care model, Australia must seek early intervention and prevention, as well as treatment of disease and illness.
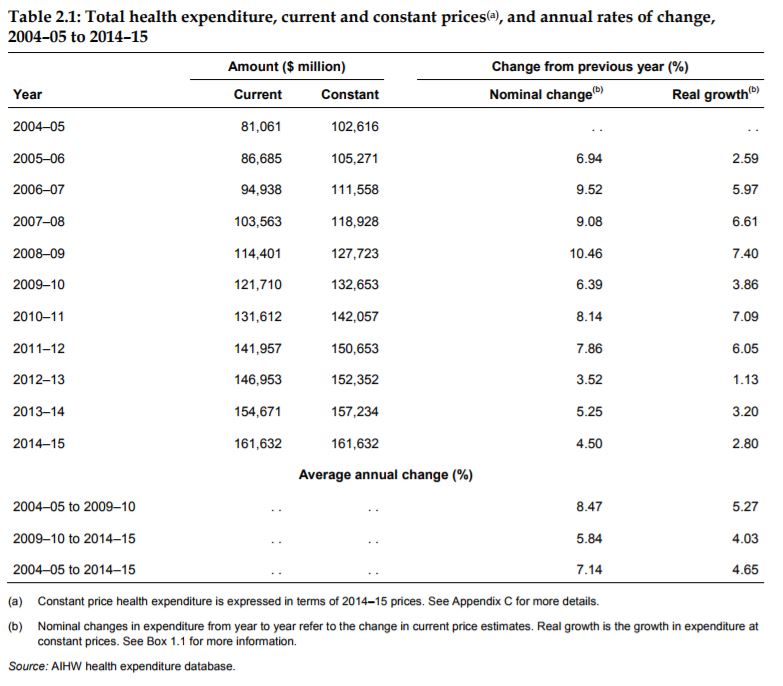
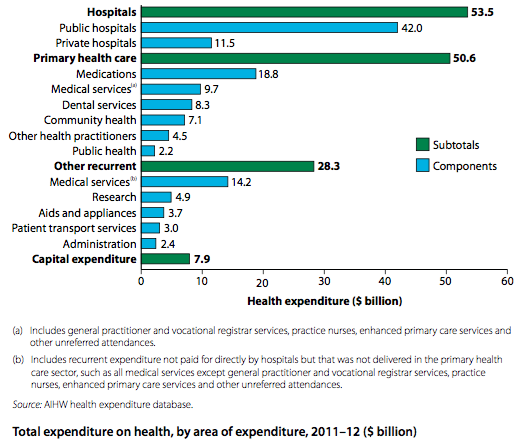
Australia spends over $160 billion dollars a year on health care and rising (not including money lost by work absence etc). The cost of health care is a large burden on the government’s expenses, early intervention and prevention can help reduce this cost. Health care expenditure currently falls into one of four areas: Hospital (38%), primary health care (36%), other recurrent expenditure (20%), and capital (6%).
Hospital refers to all costs in both public and private hospitals. Primary health care is designed to be the front line of health care and includes: GPs, nurses, allied health, and dental services. Other recurrent expenditure includes other medical services outside GPs and hospitals, research and patient transport. Capital expenditure refers to health infrastructure (building, updating and developing health care facilities see www.hinfra.health.nsw.gov.au).
Prevention refers to ‘approaches and activities aimed at reducing the likelihood that a disease or disorder will affect an individual, interrupting or slowing the progress of the disorder or reducing disability’ (WHO 2004) As such prevention includes intervention, but for the sake of the syllabus, we will address them separately.
Major prevention activities include: good hygiene, safe environments, sanitation, and a good food and water supply. Australia has all of these, and their existence has greatly increased Australia’s health over the last 100 years.
Currently, there is a focus on the increase in chronic diseases, so prevention in Australia seeks to improve lifestyle choices in relation to health. This focus aims to: decrease smoking, increase physical activity, decrease alcohol and drug use, and increase fruit and vegetable intake (healthy balanced diet).
In doing this, Australia has recognised the importance of the determinants of health and seek to create an environment conducive to good health, and address any aspects possible in the sociocultural and socioeconomic determinants of health, such as reducing costs (Medicare) and improving access to services (translators and multi-language health brochures etc).
Australia has many health promotion campaigns, some are behavioural and others are educational. They include: Life. Be In It; Slip, Slop, Slap; Every cigarette is doing you damage; and Go for 2 & 5. Other policies and regulations include: fluoridated water, seat belts in cars, plain packaging for cigarettes, and mass immunisations. The main early intervention strategy currently used in Australia is cancer-screening programs (breast, prostate, skin etc),
Preventative and early intervention strategies (prevention, protection & promotion) within the health sector cost the Australia $2.2 billion a year. This is 1.4% of total health expenditure, with the main expenses going to immunisations, health promotion and cancer screening programs.[1] Australia’s expenses on prevention and early intervention are amongst the lowest in the developed world, with New Zealand at the top spending 7% of its health budget on prevention and early intervention.
Prevention and early intervention have a great impact on quality of life, and life expectancy as well as decreasing the burden on the health care system making it a healthier workforce boosting economic performance and productivity.
Making a decision about early intervention and prevention strategies often comes down to cost and health benefits. Cost should be kept low, while gains in health should be high. Health promotion directed at large population groups are expensive, compared to specific population groups with specific risk factors.
Before interventions are undertaken, they should demonstrate value for money with economic evaluations. Cost-effectiveness compares estimated cost with potential for health improvement. This comparison, however, is difficult to demonstrate over time, making decisions difficult to make. An example of this difficulty comes with discussion over taxing food with poor nutrition and using generic drugs on combined risk factors to help prevent obesity and improving health. Vos et al (2010) concluded this was cost-saving, while Crovle & Turner (2010) showed there was a lack of long-term evaluation to verify the cost-effective claims.
The WHO (2013) has a list of ‘best buy’ policies they suggest be implemented in primary care settings in all countries. These include: reducing the impact of tobacco smoke (including no-smoking in public places), warning about tobacco danger, restricting/banning advertising for tobacco and alcohol, tax tobacco and alcohol, restricting access to alcohol, reducing salt intake, replacing trans-fats with unsaturated fats in foods, promoting awareness of good diet and exercise levels, and cancer screenings.
[1] Australia’s Health 2016 “Preventing and treating ill health”
For more info see AIHW, Australia’s Health 2014 pp341-353 AND Health expenditure Australia 2014–15