The nature of the problem
Cancer refers to cells that have become abnormal and begin to multiply rapidly and cannot be controlled by the body. Most times the body’s immune system controls abnormal cells and removes them, but some times it cannot be controlled. Cancer cells invade surrounding tissues and can be deadly. Often to help minimise the damage the body places the multiplying abnormal cells into a sack, called a tumour. Tumours can be both benign (non-cancerous) and malignant (cancerous), where malignant tumours contain cells that grow out of control and can invade surrounding tissue. Sometimes cancer moves away from the original or primary site to other sites and organs of the body. This is referred to as metastasis or secondary cancer. There are multiple cancers, most of which are named according to their location in the body – skin, lung, prostate, bowel, cervical etc. If the cancer moves to a secondary site it maintains its original site name, e.g. skin cancer that has spread to the lymph glands is still called skin cancer.

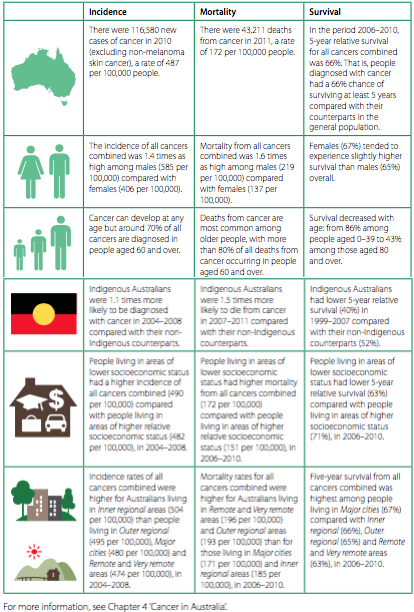
Extent of the problem (trends)
Cancer is the leading cause of death in Australia, despite survival rates improving and death rates declining. The probability of being diagnosed with a cancer before 85 is 1 in 2 for males and 1 in 3 for females. The main cancers in Australia are: prostate, bowel, breast, skin and lung cancers.
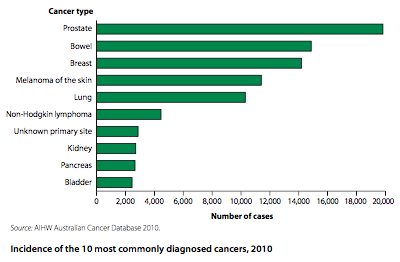
Current trends in Australia for cancer are: increased incidence, increased survival, and decreased death rates, resulting in an increase in cancer prevalence, though there is still only 3.6% of the population who have been diagnosed with cancer. The increased incidence rate is mostly due to increased detection of prostate, bowel and breast cancers.
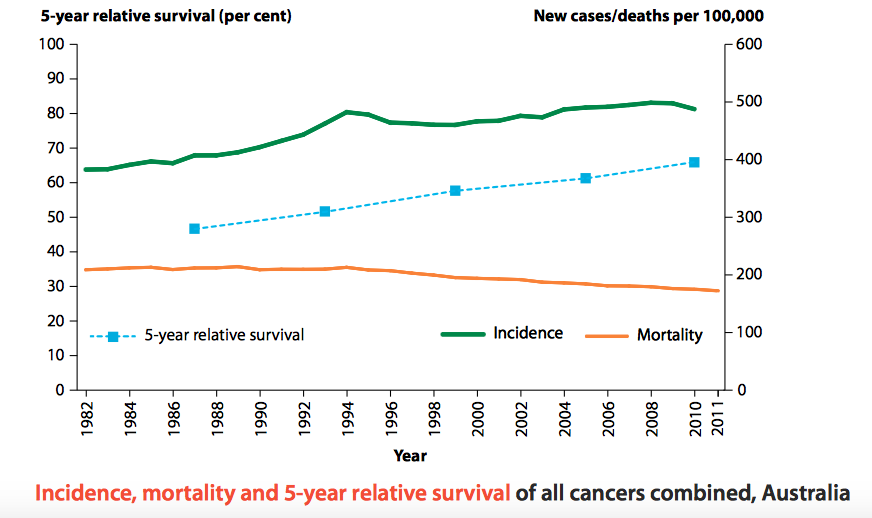
The risk of dying from cancer is 1 in 4 for males and 1 in 6 for females. The cancers with the highest mortality rates were: lung, bowel, prostate, breast and pancreatic cancer. In the last 20 years mortality rates from cancer have fallen 17%. People diagnosed with cancer have a 66% chance of surviving 5 years, 91% of people who survive the first 5 years will survive the next 5. The greatest survival gains are for prostate and kidney cancers.
Lung cancer incidence is on the decline for men, but has been increases for females. This is mostly due to the decreased smoking rates amongst men, which begun later for women.
The incidence of melanoma (main skin cancer) has almost halved over the last 30 years dropping from 5% to 2.8%. This drop is mostly attributed to greater awareness and better behavioural choices regarding UV exposure.
Breast cancer incidence has risen since the introduction of breast screening in 1992, but mortality rates from breast cancer have steadily declined and survival rates of improved.
Bowel cancer is on the decrease in Australia reducing by 1/3 from 3% to 2%. This decline is mostly attributed to a decrease in the prevalence of the bacterium Helicobacter pylori, and decreased smoking rates.
Risk factors and protective factors
The cause of most cancers is still debated, though there is growing awareness that chronic inflammation is associated with the production of abnormal cancer cells. There are a number of factors that are well recognised as risk factors for cancer:
- Behavioural factors such as tobacco smoking, alcohol, diet, obesity and physical inactivity
- Tobacco smoking is the largest single risk factor for lung cancer in Australia – causing about 90% of lung cancers in males and 65% in females (AIHW: Ridolfo & Stevenson 2001)
- The major causes of stomach cancer are the bacterium Helicobacter pylori, poor nutrition and smoking.
- Family history, genetic susceptibility and reproductive and hormonal factors
- Women with a family history of breast cancer are more likely to be diagnosed with breast cancer.
- Occupational and environmental exposures (for example, radiation, asbestos, ultraviolet light and chronic infection)
- Ultraviolet radiation is the leading risk factor for melanoma of the skin.
- Medical and iatrogenic factors (AIHW & AACR 2012; IARC 2008; WCRF & AICR 2007).
- chronic infection with the human papillomavirus (HPV) is associated with around 70–80% of all cervical cancers (Brotherton 2008).
Protective factors for cancers include:
- HPV vaccination helps prevent pre-cervical cancer lesions in young women (Gertig et al. 2013).
- Screening tests for breast, cervical and bowel cancer increase the survival rate and decrease mortality rates for the cancer as early detection improves outcomes of treatment. (BreastScreen Australia introduced in 1991 & National Bowel Cancer Screening Program introduced in 2006).
- Prostate examinations help early detection and increase the success of treatment for prostate cancer.
- Balanced diet, high in vegetables and fruit help reduce the probability of most cancers.
- Being sun-smart and not using solariums helps reduce the risk of melanoma of the skin.
The sociocultural, socioeconomic and environmental determinants
Sociocultural determinants of cancer include: family, peers, media, culture and religion. The Australian culture has often revolved around the heat of summer, beaches and getting a tan. However, recent educational actions, including advertising in the media have helped Australians know sun exposure increases the risk of melanoma of the skin. Genetics are inherited through family lines, and a history of cancer in the family increases the risk of cancer diagnosis. Other behavioural risk factors can also be affected by family and peers as people who have family and friends who smoke or are sedentary are more likely to adopt these lifestyle choices.
Socioeconomic determinants of cancer include: employment, education and income. People who have lower levels of education have lower levels of health literacy and are les aware of the risk factors and protective factors for a range of cancers. Lower levels of education also limit opportunities for employment. People who work outside have greater exposure to the sun, which places them at higher risk for skin cancers. People who work with other known sources of radiation, such as X-ray or are around electromagnetic fields frequently also have higher risk of cancer. Income can restrict access to some health services, especially some specialists. People with lower socioeconomic status have higher rates of cancer and higher mortality rates for cancer when compared to other Australians.
Environmental determinants of cancer include: geographic location and access to health services and technology. People living in rural and remote areas have higher mortality rates than other Australians. This is connected with their lack of access to specialists in cancer and less technology being available for treatment. Often rural and remote people need to travel to a major city for come cancer treatments. People who live on the beach are more inclined to be outside in the sun, which places them at more risk of some cancers.
Groups at risk
Groups at risk of cancer include:
- The elderly – 70% of diagnosis and 80% of cancer deaths were in people over 60 years of age.
- Males – cancer incidence was 1.4 times higher among males and death rates were 1.6 times higher than females.
- ATSI – are 10% more likely to be diagnosed and have 50% higher mortality rates from cancer.
- Low SES – had higher rates of all cancers and higher death rates.
- Rural and remote people – have higher mortality rates than other Australian from all cancers, though their incidence is lower.