Nature and Extent of the health inequities
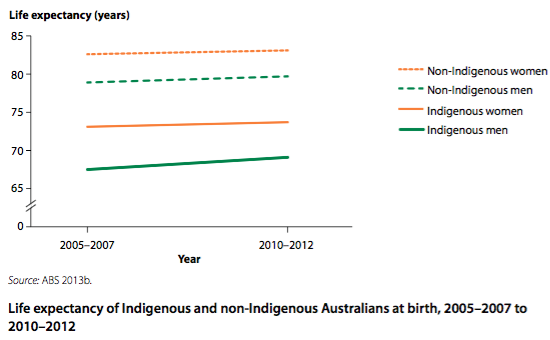
ATSI peoples experience the largest gap in health outcomes in Australia. They currently have a life expectancy 10 years lower than other Australians. Though this life expectancy is on the increase, the gap does not seem to be shrinking. Please note, that while the graph below is data from 2012, things have not changed. All life expectancy is trending upwards but the gap remains around 10 years.
The ATSI people have higher death rates in each age group than other Australians, though this is improving and the gap is decreasing. The ATSI death rate at 35-44 is four (4) times, and the child death rate is twice that of other Australians. The extent of this gap is decreasing.
ATSI people also suffer from larger death rates from circulatory diseases, endocrine, metabolic, and nutritional disorders, with an emphasis in diabetes. ATSI people are 5 times more likely to die from endocrine, metabolic, and nutritional disorders than other Australians and more likely to die of digestive conditions.
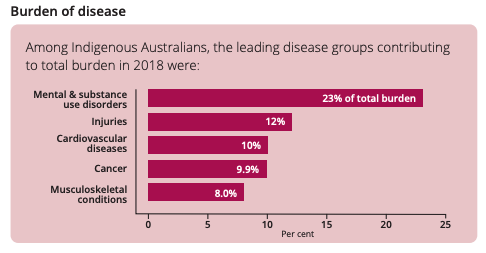
ATSI people are also more likely to suffer from long term health conditions. The current leading cause of disease burden is mental health and substance disorders.
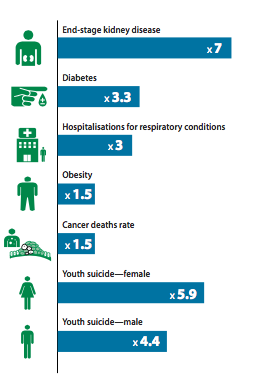
Overall ATSI people have an extensive gap in health outcomes compared with other Australians. This includes 7 times more kidney disease, 3 times more diabetes, 1.5 times more obesity and cancer death rates as well as a youth suicide rate that is 6 times more for females and 4 times more for males. ATSI people are more likely to require assistant with daily living activities as reported in the 2011 census, particularly in the under 65 age groups. There are also large gaps in self-purported mental health.
The sociocultural, socioeconomic and environmental determinants
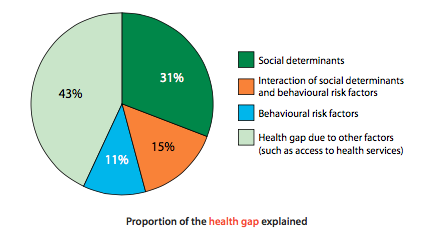
There are multiple determinants of this gap in health outcomes between ATSI and other Australians. Australia’s Health 2014 report states:
“Many factors contribute to the gap between Indigenous and non-Indigenous health. Social disadvantage, such as lower education and employment rates, is a factor, as well as higher smoking rates, poor nutrition, physical inactivity and poor access to health services.”[1]
These determinants interact with each other to produce the gap in health outcomes.
Sociocultural determinants
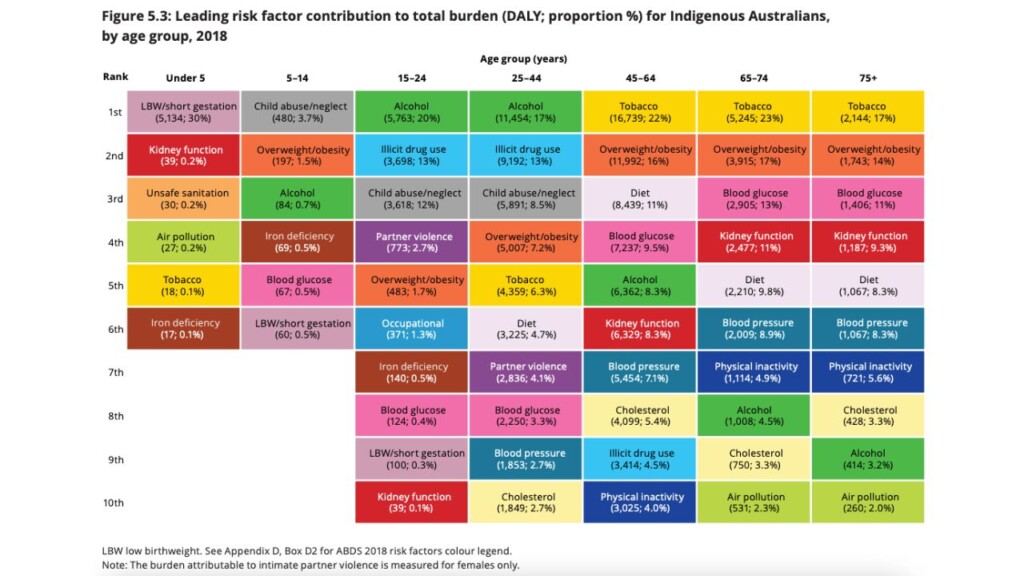
The sociocultural determinants of health for ATSI include: family, peers, religion, culture and media. Epidemiological data reveals ATSI families are less educated and have less money, which contribute to the family upbringing. There are also higher rates of domestic violence, as can be seen in the above image where child abuse/neglect is high for people aged between 5 and 44. Indigenous Australians are more likely to be imprisoned and have . Almost half of Indigenous families with dependent children are one‑parent families and 42.2 per cent of children in out-of-home care were Aboriginal and Torres Strait Islander children in 2021.
Together these statistics show the affects of sociocultural determinants on ATSI health. As ATSI are brought up in these communities and are greatly influenced by this culture. This also creates poor assess to health services with language barriers existing in some instances and poor examples being set by adults.
Another major barrier within the culture of ATSI people is the disempowerment they feel as a result of many years of oppression and discrimination from non-indigenous Australians. This ranges from the invasion of the first fleet to our white Australia policy, the stolen generation and general caricature’s of the ATSI people today. Although the Rudd Government and their Apology in 2008 went a long way towards beginning the healing process, much work is yet to be done. Tara Raven in the Australian 29 August 2008 reports that the Rudd governments intervention into child protection further disempowered the ATSI people group and causes mistrust between ATSI people and the government.
Socioeconomic determinants
The socioeconomic determinants of health include: education, employment and income. Only 51% of working-age ATSI people were employed in 2016, compared with 76% of non-Indigenous Australians. ATSI households are nearly 2.5 times as likely to be in the lowest income bracket and 4 times less likely to be in the top income bracket as non-Indigenous households. Nearly half of all Indigenous children are living in jobless families, which is 3 times the proportion of all children. Socioeconomic determinants, such as: unemployment and poorer levels of education lead not only to poor behavioural choices but also to poorer mental health conditions.
Household income, level of education, and employment status has very large impacts on health outcomes and contribute to the health gap. As do behavioural factors such as smoking, BMI, and drinking.
Environmental determinants
Environmental determinants include geographical location and access to health services and technology. Amongst ATSI people access to health services is poorer than other Australians, contributing to the gap in health outcomes. ATSI people reported having difficulty accessing health services such as dentists and GPs due to long waiting times or the services being unavailable. ATSI have higher rates of renting compared to owning a house, higher rates of homelessness and are more likely to live in rural or remote locations because of their culture. Around 1 in 5 Aboriginal and Torres Strait Islander people are living in housing that is “run down” (i.e. with major cracks, broken plumbing, no electricity) or overcrowded.
The roles of individuals, communities and governments in addressing the health inequities
Individuals are empowered by a number of interventions to make informed choices about their own behaviour and encouraged to reduce risk behaviours and increase protective behaviours. Each individual is responsible to promote their own health and the health of others
Communities and leaders of ATSI people were and are still involved in the design and implementation of many of the closing the gap programs and interventions. This includes many community groups such as Australian indigenous Doctors Association, National Aboriginal Community Controlled Health organisation, Aboriginal Community Controlled Health Services and Aboriginal Medical Services.
The Australian Government’s main role is larger health promotion and funding. The $805 million Indigenous Chronic Disease Package, is an example, and aims to improve the way the health-care system prevents, treats and manages the chronic diseases that affect many Indigenous Australians. The goal is to reduce key risk factors for chronic disease in the Indigenous community (such as smoking), improve chronic disease management and follow-up, and increase the capacity of the primary care workforce to deliver effective care to Indigenous Australians with chronic diseases (Department of Health 2013a).
The Close the Gap initiative is a statement of intent signed by Australia’s governments (state, territory & commonwealth). This statement aims to achieve equality in health status by reducing infant mortality, and increasing life expectancy in ATSI people. The statement also includes closing the gap in education, and employment outcomes; along with improving accessibility of health care to ATSI people living in remote areas. And includes specifically designed and implemented programs to address risk taking behaviours of individuals. Close the gap includes a housing strategy to improve their environmental determinant of health. Some other initiatives include: Office of Aboriginal and Torres Strait Islander Health and Aboriginal Health & medical Research Council.
You can learn more about how Australia is going in achieving the close the gap targets by searching for the latest “close the gap data compilation report” or the “Close the gap – Prime Ministers report”.
Sources
Australia’s Health 2020.
AIHW ATSI Health Performance framework data & tables.
Closing the Gap Annual Data Compilation Report July 2022
Last updated 07/2022
